By guest blogger, Kathleen Kiefer, OTR/L, HealthPartners Center for Memory & Aging
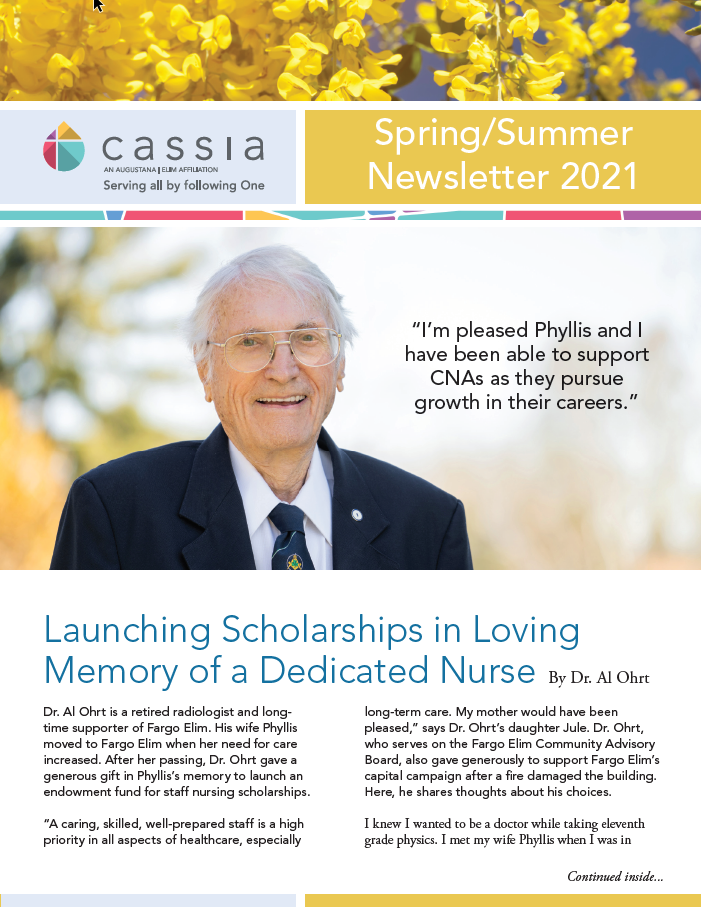
Between 1980 and 1990, it became evident that there was an increasing number of people with Alzheimer’s disease and other memory disorders. The devastating impact of Alzheimer’s on patients and their families is known to all of us. During that time, the Alzheimer’s Research Center at the HealthPartners Center for Memory & Aging in Regions Hospital began to develop new approaches to treating, preventing and caring for individuals with memory disorders. The HealthPartners Center for Memory & Aging offers information presentations sponsored by the Hopkins ACT on Alzheimer’s and Emerald Crest. We recently reached out to Kathleen Kiefer and asked her to share her insight on the subject of driving following a diagnosis of dementia.
After a loved one has been diagnosed with dementia, family and friends will often worry whether the person needs to retire from driving. As difficult as this conversation may be, it’s an important one to have. By proactively discussing driving after dementia, families can reduce the risk of unfortunate traffic accidents.
It’s important to remember that just because a loved one has been diagnosed with dementia, it doesn’t mean they’ll have to hang up the keys for good. In cases of very mild to mild dementia, patients may continue to drive safely. But someone with moderate to severe dementia, should be evaluated by a certified driver rehabilitation therapist, which is a specially trained type of occupational therapist.
Family or friends are key to starting the driving evaluation process for their loved one. If a person is experiencing any of the following, a driving evaluation should be considered:
- Difficulty with daily functioning, like meal preparation, money or medication management
- Forgetting conversations, repeating oneself or having a hard time finding words in conversation
- Visible changes in driving skills that clearly impact their safety or the safety of others, including driving too slow, near-misses or car accidents, or getting lost
- Inability to explain dents or scratches on a vehicle, or other vehicle-related mishaps like leaving a car running while unattended
Of course, if ever you or friends start to worry about your loved one driving alone or with others, such as grandkids, then you should bring up the topic of a driving evaluation.
Driving Evaluation
The occupational therapy department at Regions Hospital has collaborated with the Minnesota Department of Public Safety to create a driving school which includes a modified car to help assess driving competency. The first phase of this assessment is a pre-driving clinical screen. It is covered by medical insurance and takes place at the HealthPartners Neuroscience Center in St. Paul, MN. The screening begins with a patient and family interview, where everyone is asked about their observations and concerns. Then, the certified driver rehabilitation therapist will ask the patient specific questions. Ideally, a family member will remain in the room for this Q&A session but if the patient is more comfortable without their family member present, the family member will be asked to wait in the lobby until the pre-clinical assessment is complete. After the Q&A with a therapist, patients will also take a paper test, along with a vision test and short driving simulation. All of this information will help determine whether the patient needs a behind the wheel evaluation.
If the care team decides the patient needs a behind-the-wheel driving evaluation, it is scheduled for a later date. This is not covered by insurance and the cost is $275.
An occupational therapist will drive to the patient’s community, then allow the patient to drive the test car. The therapist will observe the driving performance for about 1.5 hours. After the evaluation, the therapist makes a final recommendation based on numerous factors, such as how well the patient obeyed traffic laws, their awareness on the road, understanding of direction and relation to home.
These recommendations can either be: no change in driving, restricted driving, or driving retirement. Although the therapist may pass the patient at that time, they are reminded that driving skills and ability could change so future evaluations will be necessary.
It is important to understand that driving safety will need to be a routine discussion with family, caregivers and health care providers. Try to find someone who is compassionate and trusted to start the conversation. In some cases, a health care clinician – like a primary care doctor – may be the best person to start discussing the topic. Relying on the expertise of a professional removes the burden from the family when making these hard decisions. The caregiver can refer back to the conversations with the health care professional when their loved one feels frustration or disappointment. After all, this is about a disease progression. The caregiver may need to repeat the decision and anticipate numerous, short conversations about it as it may tend to upset the person.
Starting the process early allows the person to begin transitioning driving responsibilities to others and finding new methods early. To see a list of the talks we give about driving, dementia and other related topics, visit us at https://www.facebook.com/fightmemoryloss/. To see a list of transportation and other resources click here. To learn more about Alzheimer’s disease visit: www.alzheimersinfo.org.
Kathleen Kiefer, OTR/L, CDRS, LDI HealthPartners Center for Memory & Aging, is a clinical specialist in rehabilitation at Regions Hospital in St. Paul, Minnesota. She graduated with a Bachelor of Science degree the University of Wisconsin – Madison in 1985. She has worked in hospital-based rehabilitation for over 25 years. She has been at Regions Hospital for 20 years and prior to that worked as a staff occupational therapist at the University of MN Hospital. In 2002 she focused her efforts on outpatient programming and eventually developed a comprehensive driving program including behind the wheel evaluation and training.